c/o involuntary movements of head since 3 yrs, c/o back pain and right knee pain since 2 years
This is an a online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan
The patient/ attender was informed the purpose of the information being acquired. An informed consent was taken from patient/ attender and there is omission of information that was requested to be omitted.
Cheif complaints:
Patient came with C/o involuntary movements of head since 3 years
Back pain since 2 years
Right knee pain since 2 years
History of presenting illness:-
A 65 year old female eho was apparently asymptomatic 3 years back and then developed involuntary movements of head, insidious in onset, gradually progressive, continuous , increased with walking and relieved with medication
Low back pain since 2 years, insidious in onset and gradually progressive, non radiating, not associated with tingling and numbness, right knee pain since 2 years, non radiating, not associated with tingling and numbness, relieved with medication
No h/o headache , fever , vomitings, chest pain, breathlessness, syncope, palpitations, no h/o burning micturition
Not a known case of DM, HTN, epilepsy, asthama, CAD,CVD, thyroid disorders
Personal history:
Diet:mixed
Appetite:normal
Sleep : normal
Bowel and bladder: regular
Micturition: burning
H/o no addiction
Family history: not significant
General examination:
Pt is c/c/c moderately nourished and built
No pallor, icterus , cyanosis, clubbing, edema,lymphadenopathy
Vitals :-
Bp : 110/70mmhg
Pr: 82bpm
Rr: 17
Grbs : 129mg/ dl
Cvs : s1 s2 heard
Rs : bae +, nvbs
P/ a : soft non tender
Cns : hmf +
Cns tone RT LT
Ul. N. N
Ll. N. N
Power. RT LT
UL. 5/5 5/5
LL. 4/5 5/5
Reflex:
B +2 +2
T +2. +2
S +1 +1
K +2 +2
A - -
P F F
Rombergs : negative
Dysdidokinesia :- negative
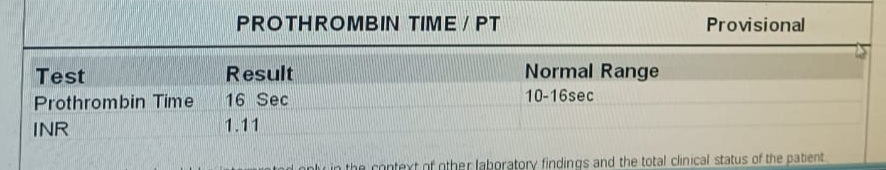
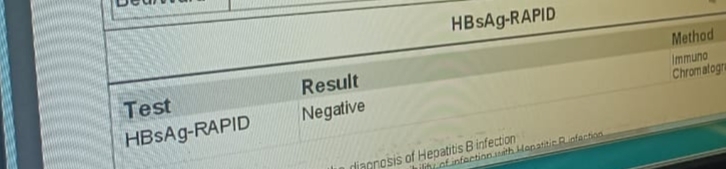
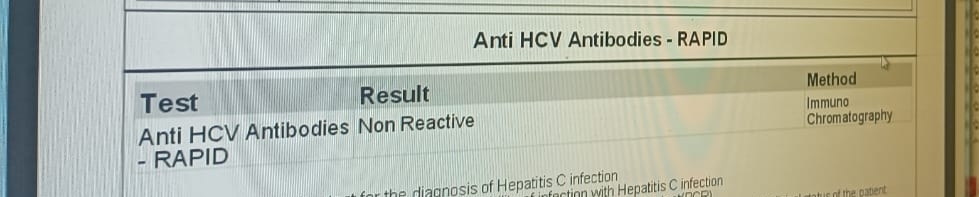
Reports :-
Provisional diagnosis: ? Atypical Parkinsonism
Treatment:
Tab.pacitane 2mg po od
Tab.pcm 500 mg po bd
Tab.supradyn po od





















Comments
Post a Comment